Venous disease is a widespread but often misunderstood condition affecting millions worldwide. Among the various manifestations of venous disease, venous insufficiency and venous ulcers stand out due to their significant impact on a patient’s quality of life. Understanding the causes, symptoms, and treatment options for these conditions is crucial in managing them effectively and improving patient outcomes.
What Is Venous Insufficiency?
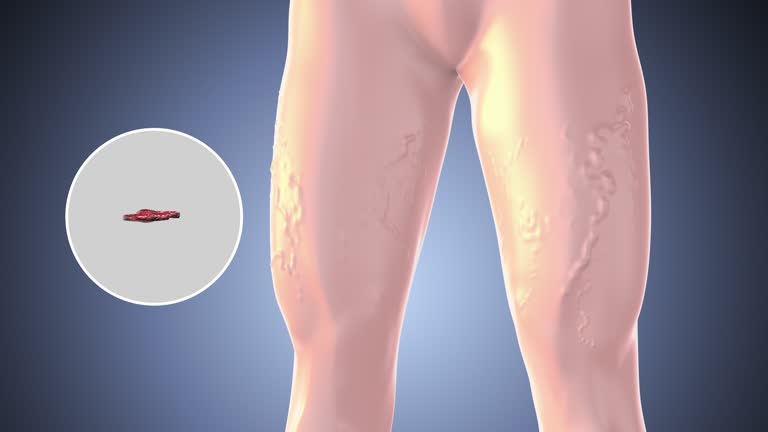
Venous insufficiency occurs when the veins in the legs are unable to pump blood back to the heart effectively. This condition often results from the weakening or damage of the valves within the veins, which are responsible for ensuring one-way blood flow. When these valves fail, blood begins to pool in the legs, leading to various symptoms that can range from mild discomfort to severe complications.
Causes of Venous Insufficiency
Several factors contribute to the development of venous insufficiency, including:
- Prolonged Standing or Sitting: Occupations that require long periods of standing or sitting can increase pressure in the veins, weakening the valves over time.
- Age: Aging naturally weakens vein walls and valves, making older adults more susceptible to venous insufficiency.
- Genetics: A family history of venous insufficiency can increase an individual’s risk of developing the condition.
- Obesity: Excess weight puts additional pressure on the veins, exacerbating valve damage.
- Pregnancy: Hormonal changes and the increased blood volume during pregnancy can strain the venous system, leading to temporary or sometimes chronic venous insufficiency.
Symptoms of Venous Insufficiency
The symptoms of venous insufficiency can vary depending on the severity of the condition. Common symptoms include:
- Swelling in the legs or ankles
- A feeling of heaviness or tiredness in the legs
- Varicose veins
- Skin changes, such as discoloration or thickening
- Pain or cramping in the legs, especially after long periods of standing or sitting
If left untreated, venous insufficiency can lead to more severe complications, such as venous ulcers.

Understanding Venous Ulcers
Venous ulcers, also known as stasis ulcers, are open sores that typically develop on the lower legs, particularly around the ankles. They are often the result of chronic venous insufficiency and represent the most severe stage of venous disease.
Causes of Venous Ulcers
Venous ulcers occur when prolonged venous insufficiency leads to increased pressure and swelling in the legs. This pressure can cause small blood vessels in the skin to burst, leading to tissue breakdown and the formation of an ulcer. Factors that increase the risk of venous ulcers include:
- Unmanaged Venous Insufficiency: Chronic venous insufficiency that is not adequately treated can lead to the development of ulcers.
- Trauma or Injury: Even minor injuries to the skin can fail to heal properly in individuals with venous insufficiency, leading to ulceration.
- Poor Circulation: Conditions that impair blood circulation, such as diabetes or peripheral artery disease, can exacerbate the risk of venous ulcers.

Treatment Options for Venous Insufficiency and Venous Ulcers
Early diagnosis and treatment are critical in managing venous insufficiency and preventing complications like venous ulcers. Treatment options include:
- Compression Therapy: Wearing compression stockings is often the first line of defense. They help improve blood flow, reduce swelling, and prevent the progression of venous disease.
- Lifestyle Changes: Regular exercise, weight management, and elevating the legs can significantly reduce symptoms and slow disease progression.
- Medications: In some cases, medications may be prescribed to improve blood flow or reduce swelling.
- Minimally Invasive Procedures: For more severe cases, procedures such as sclerotherapy, laser therapy, or vein ablation may be recommended to close or remove damaged veins.
- Wound Care for Venous Ulcers: Treating venous ulcers often involves specialized wound care to promote healing, including cleaning, dressing, and sometimes debridement of the ulcer. In some cases, skin grafts may be necessary.
Preventing Venous Disease
Venous disease, including conditions like venous insufficiency and varicose veins, can significantly impact your quality of life if not managed effectively. Prevention is key to minimizing your risk and maintaining optimal vascular health.
Below are proven-to-work tips and strategies to help you prevent venous disease.
Maintain an Active Lifestyle
Regular physical activity is crucial for preventing venous disease. Exercise helps improve circulation, reducing the risk of blood pooling in the veins, which can lead to varicose veins and other complications.
Aim for at least 150 minutes of moderate exercise per week, such as walking, swimming, or cycling. Incorporate muscle-strengthening activities twice a week to enhance vascular health further.
Healthy Weight Management
Carrying excess weight puts additional pressure on your veins, particularly in the lower extremities, increasing your risk of venous insufficiency. Maintaining a healthy weight through a balanced diet and regular exercise is essential for reducing this strain on your veins.
Dietary Considerations
A diet rich in fruits, vegetables, whole grains, and lean proteins can support vascular health. Limiting salt intake is particularly important, as excessive salt can lead to fluid retention, which exacerbates venous issues. Additionally, foods high in fiber help prevent constipation, reducing the strain on your veins during bowel movements.
Avoid Prolonged Sitting or Standing
Long periods of sitting or standing can hinder blood flow, leading to venous stasis. If your job requires prolonged periods in one position, make it a point to move around every 30 minutes. Simple actions like stretching your legs, walking a few steps, or flexing your calf muscles can make a significant difference in preventing venous issues.
Proper Footwear Choices
Wearing low-heeled shoes encourages better calf muscle function, which is essential for blood circulation in the legs. Avoid high heels as much as possible, as they limit the movement of your calf muscles, impeding blood flow.
Compression Stockings
For individuals at higher risk of venous disease, such as those with a family history or jobs that require long hours of standing, wearing compression stockings can be beneficial. These stockings help maintain blood flow and reduce swelling in the legs, preventing the development of varicose veins and other venous conditions.
Regular Medical Check-ups
Regular visits to your healthcare provider can help detect early signs of venous disease, allowing for prompt intervention. If you experience symptoms like swelling, pain, or visible veins, consult your doctor for appropriate management. Early diagnosis and treatment can prevent the progression of venous insufficiency.
Stay Hydrated
Hydration is key to maintaining healthy blood flow. Dehydration can cause blood to thicken, increasing the risk of clot formation and venous issues. Ensure you’re drinking enough water throughout the day, particularly in hot weather or after physical activity.
Mindful Posture
Avoid crossing your legs while sitting, as this can restrict blood flow. Instead, sit with your feet flat on the floor or elevate your legs when possible to encourage better circulation.
Early Mobilization Post-Surgery
If you’ve undergone surgery, especially orthopedic procedures, it’s vital to start moving as soon as it’s safe to do so. Early mobilization helps prevent blood from pooling in your veins, reducing the risk of deep vein thrombosis (DVT). Follow your healthcare provider’s recommendations for post-operative activity.

Bottom Line
Venous insufficiency and venous ulcers are significant health concerns that require prompt attention and treatment. By understanding the causes, recognizing the symptoms, and exploring the available treatment options, individuals can take proactive steps in managing venous disease and improving their quality of life.
If you or someone you know is experiencing symptoms of venous insufficiency, it’s important to seek medical advice to prevent the progression of the disease and the development of venous ulcers.
Looking to stay healthy without breaking the bank? Don’t look any further.
Subscribe to Kloud Iron’s 28-day fitness program and begin your journey toward optimal mental health and physical fitness.
To learn more about Kloud Iron Fitness Hub’s offers, contact us today or message/follow us on Facebook and Instagram. We are also available on YouTube.


1 Comment
Understanding Stasis Dermatitis: Causes, Treatment, and Prevention – Kloud Iron Fitness Hub
2 months ago[…] seen in older adults, this condition is closely linked to venous insufficiency—a disorder in which the veins struggle to send blood from the legs back to the heart. If left […]